Understanding Chronic Pain
Chronic pain, defined as pain persisting for more than three months, impacts an estimated 50 million adults in the United States alone and affects millions more worldwide. Unlike acute pain, which signals injury or illness and typically resolves as the body heals, chronic pain often continues without a clear cause or can outlast the original injury or illness. The ongoing nature of chronic pain can significantly disrupt daily activities, reduce mobility, and greatly affect mental and emotional well-being. Sufferers often experience mood swings, anxiety, depression, and social withdrawal, as the relentless nature of their pain affects every aspect of their lives. For those seeking specialized care, Pain Therapy Associates, a leading Midwest vascular pain specialist Chicago, offers comprehensive services tailored to individual needs. With multiple locations in the Chicago area, including Hoffman Estates and Portage Park, they provide expert care that addresses the complex, individualized nature of chronic pain, offering hope and support for lasting relief.
Incorporating Mindfulness and Meditation
Mindfulness and meditation have emerged as powerful non-pharmaceutical strategies for alleviating chronic pain. These mind-body practices help individuals become more aware of their physical sensations, emotions, and thoughts, thus altering the brain’s perception of discomfort. Through consistent, guided meditation or daily mindfulness practices, patients can train their minds to observe pain with less emotional reactivity and reduce the urge to catastrophize. For example, mindfulness-based stress reduction (MBSR) programs teach techniques that enable people to break the cycle of pain, anxiety, and depression, leading to improved pain tolerance and a greater sense of well-being. A 2024 review found that participants who integrated mindfulness and meditation into their routines experienced significant reductions in pain intensity, disability, and distress, reinforcing the value of these practices in comprehensive pain management.
Engaging in Regular Physical Activity
Staying physically active plays a crucial role in chronic pain management. Exercise strengthens muscles, enhances flexibility, and helps maintain joint health, all while stimulating the release of endorphins—natural chemicals in the body that fight pain and boost mood. Even gentle activities like walking, swimming, yoga, or tai chi can have substantial benefits, as they gently mobilize the body without putting excessive stress on joints and tissues. Studies consistently show that people who stick to a regular exercise regimen not only experience less pain but also enjoy better sleep, improved mobility, and reduced symptoms of anxiety and depression. Physical therapists often recommend tailored exercise programs to help individuals safely increase activity levels, reduce reliance on medication, and foster long-term resilience.
Adopting a Balanced Diet
Nutrition is a frequently overlooked but vital aspect of chronic pain management. A diet rich in anti-inflammatory foods such as fruits, vegetables, whole grains, fatty fish, nuts, and seeds can help reduce inflammation and, in some cases, alleviate pain. Omega-3 fatty acids, found in fish such as salmon and sardines, are known for their ability to help calm inflammation. At the same time, antioxidants from colorful fruits and leafy greens help neutralize harmful free radicals that can aggravate pain. Reducing processed foods, sugar, and unhealthy fats also lowers inflammation and can improve digestion and energy levels, both of which contribute to feeling better overall. Those coping with pain may also benefit from consulting a nutritionist to customize a diet plan tailored to their unique needs.
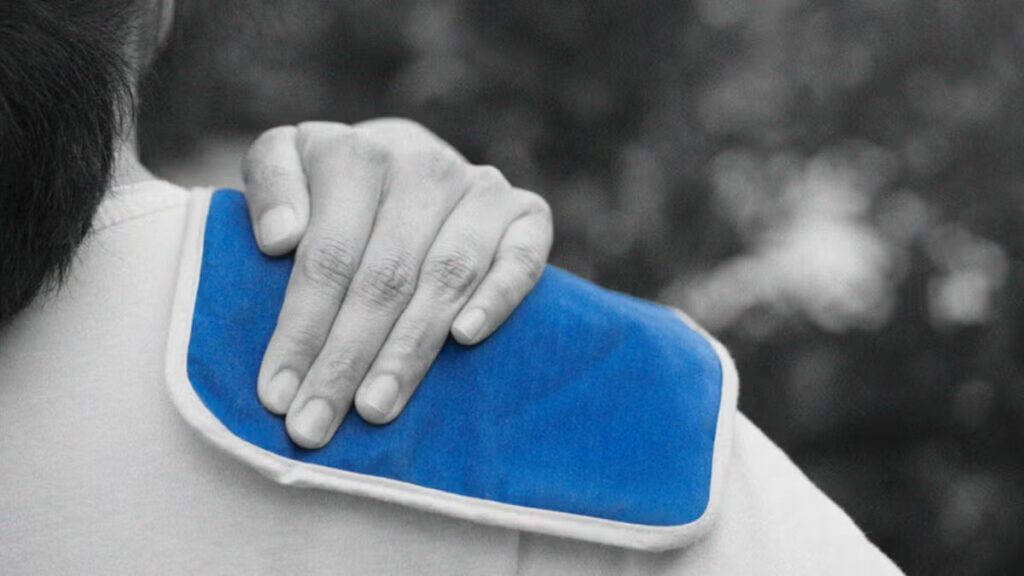
Utilizing Heat and Cold Therapy
Heat and cold therapy are simple, accessible methods for managing various types of chronic pain. Applying heat to sore areas encourages blood flow, relaxes tight muscles, and promotes healing in tissues. Heat can be especially helpful for conditions such as chronic muscle pain or stiffness, as it soothes discomfort and increases flexibility. Conversely, cold therapy, such as an ice pack or cold compress, is effective for reducing inflammation and swelling and for numbing sharp or acute pain. Both methods are often recommended as first-line home treatments and can be alternated based on symptoms. According to a 2021 survey, most people living with chronic pain regularly use heat and cold therapy as part of their daily self-care routines.
Exploring Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy, or CBT, is a psychological treatment that helps individuals identify and modify negative thoughts and behaviors associated with chronic pain. CBT interventions focus on reframing the way people think about pain, empowering them to develop healthier responses and cope more effectively. For many, the anticipation of pain or fear of increased discomfort can become overwhelming, contributing to a cycle of avoidance and reduced activity that exacerbates suffering. CBT teaches people to challenge these patterns, set realistic goals, and gradually increase their participation in meaningful activities. Studies reveal that CBT is linked to improvements in pain management, emotional resilience, sleep quality, and overall quality of life, making it a valuable tool for anyone struggling with persistent pain.
Ensuring Quality Sleep
Quality sleep is essential for those managing chronic pain, as inadequate rest can heighten pain sensitivity and hinder physical and emotional recovery. Poor sleep is known to directly worsen pain, decrease pain tolerance, and contribute to mood disorders. Establishing a regular bedtime and wake-up time, minimizing exposure to blue light from screens before bed, and creating a calm, dark, and comfortable sleeping environment are important steps toward better sleep hygiene. Relaxation techniques before bed, such as gentle stretching, meditation, or deep-breathing exercises, can help signal the body that it is time to rest, improving the likelihood of falling and staying asleep.
Seeking Professional Guidance
While self-management strategies are crucial, individualized support from healthcare providers can make a significant difference in chronic pain outcomes. A physician, pain specialist, or therapist can assess underlying causes, prescribe targeted therapies, and help patients navigate treatment options, including medication, physical therapy, and procedural interventions when necessary. Pain specialists may also coordinate multidisciplinary care, involving nutritionists, psychologists, or occupational therapists as needed. For those in the Midwest, particularly in Chicago, Pain Therapy Associates offers comprehensive, personalized services. As a leading Midwest vascular pain specialist in Chicago, they deliver expert care tailored to each patient’s unique medical and lifestyle needs, providing hope and effective long-term solutions.
By thoughtfully integrating these evidence-based strategies, individuals living with chronic pain can take proactive steps toward reducing their symptoms, reclaiming their independence, and enhancing their quality of life. Chronic pain management is a multi-faceted journey, and with the right tools, knowledge, and support, lasting relief is more attainable than ever before.